With updates coming in almost daily about dental aerosols and their risks, we’ve decided to consolidate all the global dental aerosol news in one location, with some thoughts and analysis added as to how it impacts dentists, DA’s, and Hygienists.
Come back often or subscribe on the right to be notified when updates are added to the page.
5th of October – COVID-19 is Airborne
The CDC confirmed today what many researchers have been compiling a growing body of evidence for by officially stating that COVID-19 can be airborne. This has huge implications for enclosed indoor spaces, affecting everything from public transport to most types of buildings, and particularly dental practices.
“In the healthcare setting, aerosol is used with respect to “aerosol-generating procedures” (e.g., intubation, bronchoscopy) that produce small droplets and particles and require distinct engineering controls to prevent occupational transmission of infectious pathogens like SARS-CoV-2.” – CDC Scientific Brief
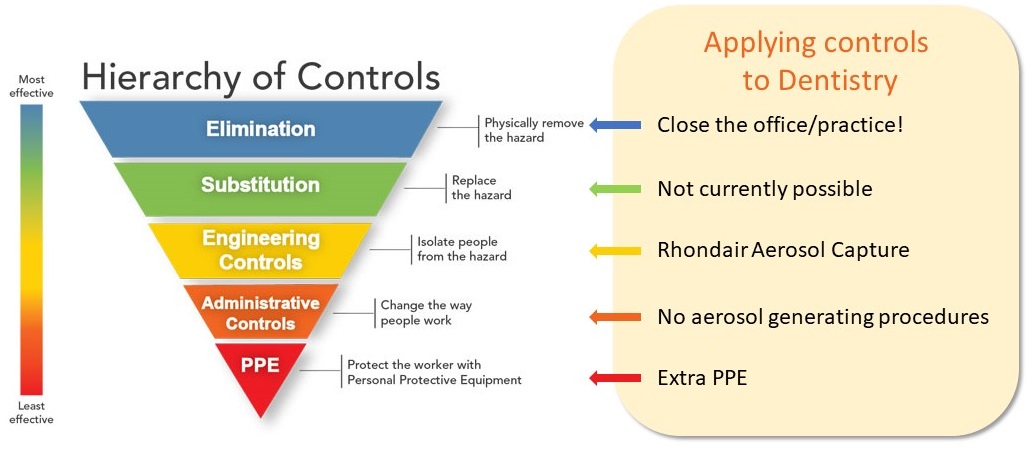
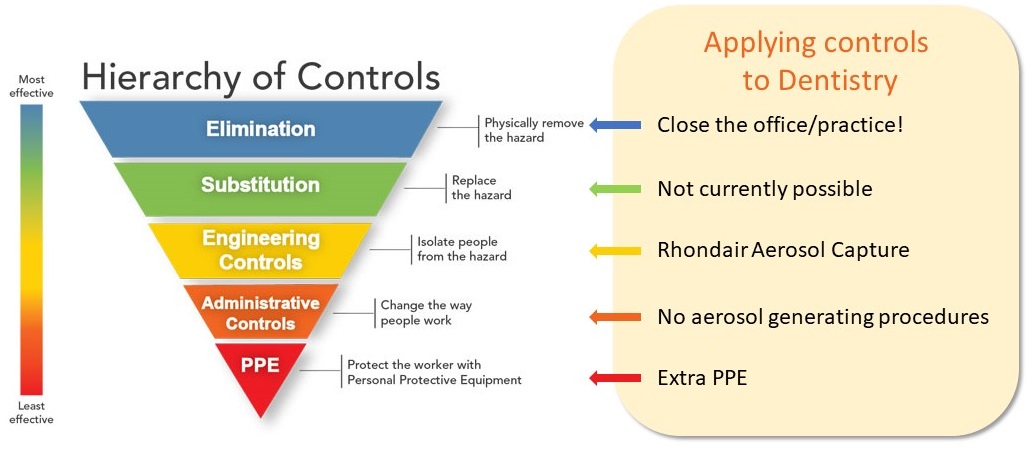
This means that aerosol generating procedures should only be performed with Engineering Controls in place, not just PPE controls like face masks. Are you unclear on the distinction between Engineering and PPE controls? We explain the differences and provide a customisable Dental Risk Management Plan template on our website.
Close proximity – less than 6ft/2m – combined with exposure lengths of 30 minutes or greater are considered the main path for infections, with reduced airflow increasing the chances. Otherwise known as the standard context for most dental appointments.
2nd of October – FGDP Updates their Guidelines
The Faculty of General Dental Practice in the UK has updated its guide for the safe management of general dental practice to provide pathways for the reduction of fallow times.
A Fallow Time Calculator has also been released to help practitioners determine the fallow time that is applicable to their situation.
When the guides were originally released, they recommended a 60-minute fallow period for many procedures with no real way to reduce the time-frame. Many in the industry at the time expressed concern that these guidelines were impractical from an operational standpoint and didn’t account for mitigation measures put in place.
While it’s good to see the feedback taken on board, the next steps should be a greater focus on the engineering controls aspect of aerosol reduction instead of a predominant reliance on PPE measures.
10th of September – Asymptomatic Patients 40% of Infections
The current best estimate by the CDC is that asymptomatic patients account for around 40% of infections. While they admit that such cases are hard to detect by their very nature, they are also considered almost as infective (75%) as a person showing symptoms.
It’s also not a stretch to see how even with a somewhat reduced infectivity, these cases could in fact be more dangerous overall in real world scenarios. Most people today showing symptoms are self-isolating, doing what they can to reduce the spread. People not showing symptoms, however, are far more likely to be out in the community. It’s also the main risk in relying on screening and temperature checks in dental practices – asymptomatic people will pass right through these tests and into the dental chair.
29th of August – CDC Advise Considering HEPA Units
Within Dentistry specifically, the CDC’s guidance for dental settings is to“consider the use of a portable high-efficiency particulate air (HEPA) air filtration unit while a patient is undergoing, and immediately following, an aerosol generating procedure.
Rather than just relying on the building’s HVAC system capacity, use a HEPA air filtration unit to reduce aerosol concentrations in the room and increase the effectiveness of the turnover time.”
Another important aspect to consider is the placement for any unit that will affect airflow. Drawing air should always be lead away from patients and healthcare personnel, without directing the flow from an individual past another, and the shortest route possible to a capture system.
Hierarchy of Controls for the Most Effective Protection Possible
The “Hierarchy of Controls” is based on established safety protocols from The National Institute for Occupational Safety and Health (NIOSH), part of the US Centers for Disease Control and Prevention (CDC). Elimination and Substitution are not viable options to keep your practice open. Engineering Controls such as source capture with air purification are the best option available.