“I just don’t feel safe spending all day in a soup of pathogens.”
That’s the feedback from a dentist we spoke to who had reopened their practice, and it’s hard to disagree with them. Dentistry is one of the most at-risk occupations for COVID-19 transmission today and dental aerosols are a near-perfect medium to spread disease.
Since the initial outbreak of the pandemic, a common theme for dental industry professional groups around the world has been a reliance on PPE as the primary control mechanism for risks. While PPE should absolutely be used, standard health and safety practice tells us that PPE is the least effective hazard control available. It’s what you rely on when all the other safety processes fall down.
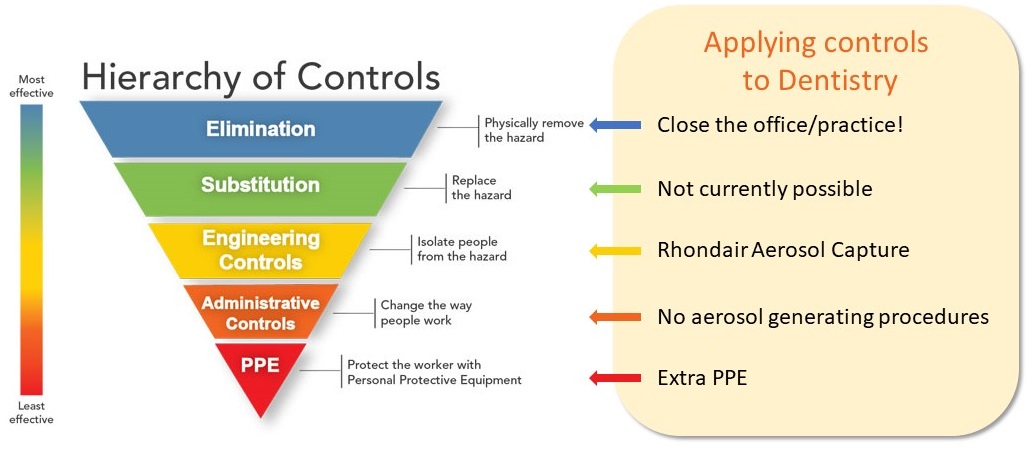
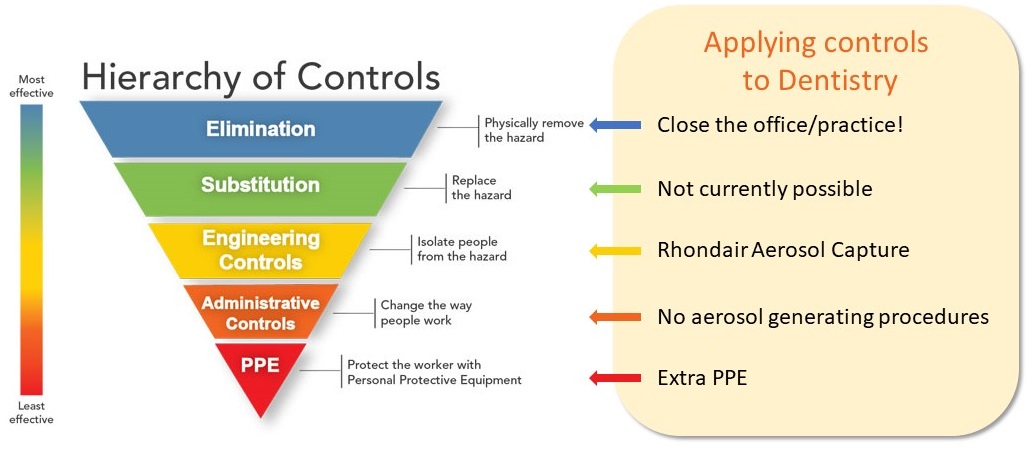
In short; PPE should be your last line of defence, not your first.
Capturing aerosols at their source is the safest control method available today.
The “Hierarchy of Controls” is based on established safety protocols from The National Institute for Occupational Safety and Health (NIOSH), part of the US Centers for Disease Control and Prevention (CDC). Elimination and Substitution are not viable options to keep your practice open. Engineering Controls such as source capture with air purification are the best option available.
The Centers for Disease Control and Prevention also urge dental practitioners to “Consider the use of a portable high-efficiency particulate air (HEPA) air filtration unit while the patient is undergoing, and immediately following, an aerosol-generating procedure.”
Another key point the CDC emphasises is the need to isolate the patient as much as possible during procedures under filtration: “Position the unit to ensure that it does not pull air into or past the breathing zone of the Dental Healthcare Practitioner.”
The Rhondair’s funnel shape and placement is specifically designed to draw aerosols away from the patient and dental practitioners while providing care.
The Rhondair Aerosol Capture System creates a barrier between the patient and the dentist to contain AGPs at the source, removing them via an industrial-strength fan and filtering the potentially harmful aerosols through a H13 HEPA filter to capture 99.95% or more of all particles – including the size ranges that viruses, COVID-19, and dental aerosols exist within.


The Smoking Gun
With the latest research from the University of Florida showing COVID-19 can survive in suspended aerosol particles, it’s now time to rethink effective hazard management.
“This is what people have been clamoring for,” said Linsey Marr, an expert in airborne spread of viruses who was not involved in the work. “It’s unambiguous evidence that there is infectious virus in aerosols.”
Recent revelations in aerosol testing methods by virologists and aerosol scientists have shown that aerosols small enough to stay suspended in the air for hours can still contain viable live virus. These results and a growing body of evidence are now forming to suggest a shift will soon be required in the dental community’s approach to keeping themselves, their staff, and their patients safe.
The journal article also shows a very important finding: The only results outside control samples to show zero viable virus cells were samples that had been through HEPA filters.
The implications of this research could be far reaching for indoor settings – effectively rendering any enclosed, populated space not using small-particle air filtering a potential hazard.
While there’s still a lot of research to be done on the virus, this is looking to be one of the biggest pieces of the puzzle now coming into view.
So what’s the answer?
To help navigate the complexities of providing safe and effective dental care, we’ve put together a Risk Management Plan template for dental aerosols.
This document can be modified to suit individual treatments offered in your practice and is focused on the two highest-risk stages of patient care in a dental setting: treatment and post-treatment.
Specific controls for all major dental processes are covered, including direct restoration, tooth polishing, periodontal and endodontic procedures, and surgical implants.
Many dentists are business owners who have a duty of care through health and safety legislation to protect their staff and themselves from injury in the workplace. One of the best ways to do this is to demonstrate they are taking a risk-based approach to understanding the key risks that could impact on their staff and have a remediation plan in place to manage or eliminate these risks.
The risk management plan can form part of your organisation’s approach to safely operating in a way that makes sense, protects you and your staff, reassures patients, and minimises your risks.
Until next time, stay safe.
The team at Rhondium.