This article was originally published in the July-August 2018 edition of the Australasian Dentist Magazine.
Restoring and strengthening badly broken-down teeth is normally achieved through the placement of indirect restorations such as multiple appointment laboratory made crowns. This article describes Rhondium’s new One Visit Crown (OVC) system. The OVC system does not require a CAD/CAM, and makes it possible to complete a full cuspal overlay restoration in one visit, taking less than an hour in total (usually about 30-45 minutes once proficient with the procedure).
The OVC crown is made of a hybrid ceramic material that has a cured occlusal surface and an uncured under-layer made of the same material. The uncured layer is moulded and customised to fit the tooth preparation. This type of material is ideal for heavily broken-down teeth as it has several advantages:
1. It is very fracture resistant when bonded to teeth.
2. It has stress absorbing characteristics therefore reducing the stress to the tooth itself (ideal for root canal treated teeth).
3. It has very high bond strength to resin cements.
4. It can be easily repaired. Even though it is less likely to fracture than porcelain, if it does fracture, the material is easy to bond to and therefore it is repairable.
5. If a root canal is required in the future, it is possible to drill through the One Visit Crown without the concern of chipping a porcelain crown and then afterwards bond a composite core/filling to fill the access hole.
6. Very aesthetic with great margin adaptation.
7. The OVC can be stained or characterised to further improve the aesthetic results.
Rhondium has shown good strength test results, and leading author Dr. Pascal Magne has done extensive research with hybrid ceramic materials showing their advantages.
Restoring broken down teeth case studies
In modern dentistry there has been a move away from full crown preps towards more conservative preparations with supra-gingival margins due to the strong bonds that can now be achieved.
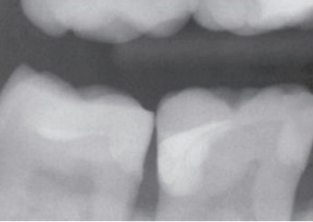
   |    |
| Case 1: Before | Case 2: After |
In this first case, the buccal cusp was overlaid by about 1.5mm and the exposed dentine tidied up. The margin was bevelled which made it disappear nicely and enhanced bonding quality. Some staining of the occlusal surface was completed for a very natural looking and conservative option – arguably more so than the PFM behind it. At the time of writing this article, this particular OVC has now been in place for over 3 years. Because the overheads are lower with the OVC and it does not require as much time to place as a conventional lab crown, the patient was charged a lower fee. Subsequently this same patient with two additional heavily broken-down teeth decided in favour of the OVC due to affordability. This patient also referred his wife specifically for the OVC procedure.
   |    |
   |    |
   | 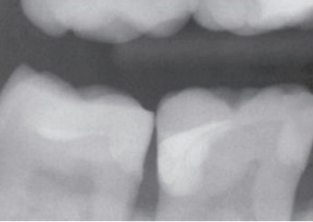 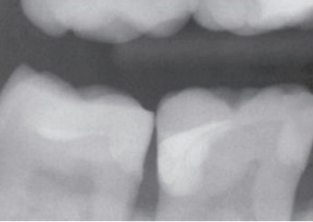  |
| Case 2 |
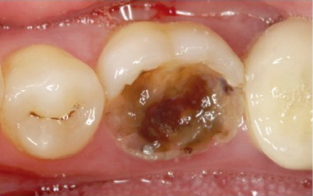
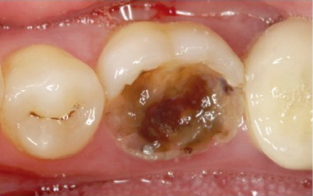
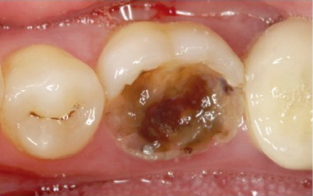
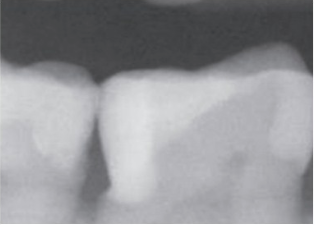
This next case, Case 2, has a very deep distal box with an old composite in place that exhibited symptoms of cracked tooth syndrome. The OVC Wedge (green) was used to fill the deep box before placing an OVC over the top. These OVC Wedges are a great tool for many situations. They simultaneously depress the gums, prevent contamination, fluid seepage and form a very nice natural tooth shape in the proximal area which makes building up deep boxes more predictable.
   |    |    |
| Case 3 |
Case 3 was a severely broken down upper premolar that had very deep subgingival decay on the mesio-palatal area. This patient opted to try and save the tooth over an extraction. The OVC was ideal due to its ease of placement and the potential requirement for root canal treatment. The hybrid ceramic material of the OVC means that it is possible to drill down through the OVC for root canal treatment without fracturing the crown. This tooth was relatively easy and quick to restore to a pleasing result and has now been in function for over three years. During the prep I was careful to allow enough tooth above the gum line to aid in matrix band retention.
   |    |
| Case 4: Before | Case 4: After |
Case 4: Here are pre-operative and post-operative images showing more OVC cases on severely decayed teeth.
   |    |
| Case 5: Before | Case 5: After |
Case 5: This case involved a tooth broken down at gum level still able to be restored with the OVC.
   |    |
| Case 6: Before | Case 6: After |
Case 6: A great solution for amalgam replacement.
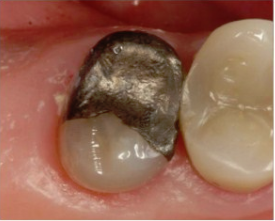 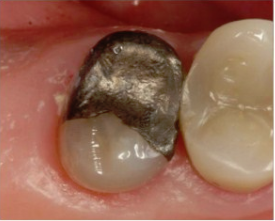 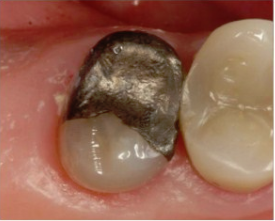 |    |
| Case 7: Before | Case 7: After |
Case 7 shows a heavily amalgam filled premolar restored with an OVC.
   |    |    |
| Case 8 |
In Case 8 the patient had been through a successful root canal treatment and was recommended a crown. The patient changed practice after finding out about the OVC and was very pleased with the relative affordability of the OVC crown and the final outcome.
Review of the One Visit Crown (OVC)
Throughout my experiences with the One Visit Crown I have had very few problems. I am aware of one de-bond on a tooth that was broken at gum level, in this case extraction was a strong option, however the patient elected the OVC. It was bonded with Panavia and de-bonded after three years. After placing over 600 OVC’s over the past five years, sometimes on very broken-down teeth, this is the only case that has de-bonded. I have found the OVC to be a great adjunct to my practice. It fills a need for many patients for a one visit, good value solution, and the high number of patient referrals has reflected the demand for it.
Learn more about the One Visit Crown CPD seminars and courses in your area at www.rhondium.co.uk. Contact Rhondium on free-phone AUS 1800 449 282 NZ 0800 746 634 or email info@rhondium.com.
About the author
Dr Adam Doudney has over 20 years clinical experience and has been a leading dentist at Lumino in New Zealand since 2007 as well as being part of the clinical advisory board for Lumino since 2014. He graduated from Otago University New Zealand with a Bachelor of Dental Surgery and also holds a Postgraduate Diploma in Business. Dr Doudney has presented and published several articles on implants, as well as being a clinical adviser for Triodent and now for Rhondium. Dr Doudney lectures extensively on One Visit Crowns in New Zealand and abroad.
To view the original article published in the July-August 2018 edition of Australasian Dentist, please visit: http://www.printgraphics.net.au/myfiles/Australasian-Dentist-July-August-2018/72/index.html
